Documentation and Administrative Tasks?
Physician burnout is a serious problem affecting doctors' and their patient's health and well-being. Burnout is characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. It can lead to increased medical errors, lower quality of care, substance abuse, depression, and suicide.
In this blog post, we will look at some of the latest statistics on physician burnout, how it varies by specialty and year, what are the costs and consequences of burnout, how it compares across different countries, and what are some of the interventions that can help prevent and reduce burnout.
According to a nationwide survey of physicians conducted by the American Medical Association (AMA), nearly 63% of physicians reported at least one symptom of burnout at the end of 2021 and the beginning of 2022. Only 30% felt satisfied with their work-life balance, compared with 43% five years earlier.
This is the biggest increase in emotional exhaustion ever seen in the literature. The survey also showed a stark contrast with the data from 2020, when only 38% of doctors reported burnout symptoms, and 46% were satisfied with their work-life balance.
The AMA survey also revealed that physician burnout varies by specialty. Some of the specialties with the highest rates of burnout in 2021-2022 were critical care (75%), rheumatology (74%), infectious diseases (72%), emergency medicine (71%), and neurology (70%). Some of the specialties with the lowest rates of burnout were ophthalmology (45%), dermatology (46%), pathology (47%), orthopedics (48%), and psychiatry (49%).
Some specialties experienced a significant increase in burnout from 2017 to 2021-2022, such as infectious diseases (from 48% to 72%), rheumatology (from 57% to 74%), nephrology (from 49% to 68%), and neurology (from 53% to 70%). Some specialties experienced a slight decrease in burnout, such as dermatology (from 50% to 46%), ophthalmology (from 48% to 45%), and pathology (from 51% to 47%).
The following table shows the burnout rates by specialty in 2021-2022 and 2017, based on the AMA survey data:
| Specialty | Burnout rate in 2017 | Burnout rate in 2021-2022 |
|---|---|---|
Critical care | 55% | 75% |
Rheumatology | 57% | 74% |
Infectious diseases | 48% | 72% |
Emergency medicine | 59% | 71% |
Neurology | 53% | 70% |
Ophthalmology | 48% | 45% |
Dermatology | 50% | 46% |
Pathology | 51% | 47% |
Orthopedics | 50% | 48% |
Psychiatry | 42% | 49% |
Another way to look at physician burnout is by comparing the trends over time. A study published in Mayo Clinic Proceedings analyzed the data from five national surveys conducted between 2011 and 2022. The study found that physician burnout increased from 45.5% in 2011 to 54.4% in 2014, decreased to 43.9% in 2017, then increased again to 62.8% in 2021-2022.
The study also found that work-life satisfaction decreased from 48.5% in 2011 to 40.9% in 2014, then increased to 42.7% in 2017, then decreased again to 29.5% in 2021-2022. The study attributed these fluctuations to various factors, such as changes in healthcare policies, regulations, technology, and practice models.
The table below summarizes the trends of physician burnout and work-life satisfaction over time:
| Year | Burnout Rate | Work-Life Satisfaction |
|---|---|---|
2011 | 45.5% | 48.5% |
2014 | 54.4% | 40.9% |
2017 | 43.9% | 42.7% |
2020 | 38.2% | 46% |
2021-2022 | 62.8% | 29.5% |
Physician burnout has significant costs and consequences for both doctors and patients. According to a study published in the Annals of Internal Medicine, physician burnout costs the U.S. healthcare system about $4.6 billion annually due to reduced productivity, increased turnover, and early retirement. Another study estimated that physician burnout costs about $7.75 million per hospital annually due to increased malpractice risk, reduced patient satisfaction, and lower quality of care.
Physician burnout also affects the health and safety of doctors and patients. A meta-analysis found that physician burnout is associated with a twofold increase in the risk of medical errors. Another meta-analysis found that physician burnout is associated with a higher risk of depression, suicidal ideation, and suicide. A survey by Medscape found that more than one-third of physicians have considered suicide at some point in their careers.
Physician burnout is not unique to the U.S. It is a global phenomenon that affects doctors in many countries. A systematic review found that the prevalence of physician burnout ranged from 0% to 80.5% across different countries, with an average of 34.6%. The review also found that some factors contributing to physician burnout are common across countries, such as workload, time pressure, lack of autonomy, lack of support, lack of resources, and lack of recognition.
However, some factors may vary by country, such as cultural norms, healthcare systems, payment models, and regulatory environments. For example, a study comparing physician burnout in the U.S. and the Netherlands found that U.S. physicians reported higher burnout, lower satisfaction, and more administrative burdens than Dutch physicians. The study attributed these differences to the differences in healthcare systems, such as the single-payer system, universal coverage, and lower costs in the Netherlands.
Another study comparing physician burnout in six European countries (France, Germany, Italy, Portugal, Spain, and the U.K.) found that the prevalence of burnout ranged from 17% in Italy to 43% in France. The study also found that some factors associated with lower burnout were higher income, more control over the work schedule, more positive feedback, and more social support.
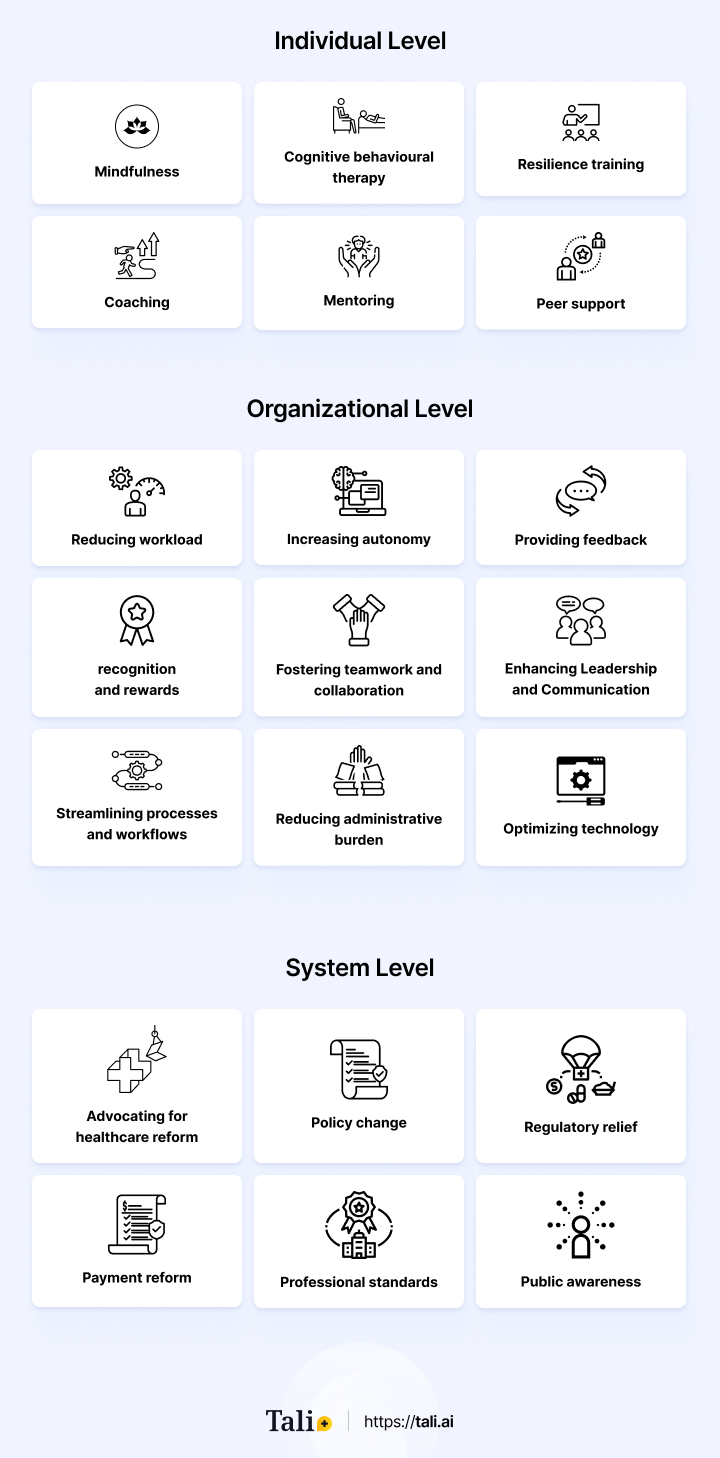
Physician burnout is a complex and multifaceted problem that requires a comprehensive and systemic approach. There is no one-size-fits-all solution, but some evidence-based interventions can help prevent and reduce physician burnout at different levels.
At the individual level, some interventions that can help physicians cope with stress and enhance well-being include:
Mindfulness
Cognitive behavioral therapy
Resilience training
Coaching
Mentoring
Peer support
At the organizational level, some interventions that can help improve the work environment and reduce the sources of burnout include:
Reducing workload
Increasing autonomy
Providing feedback, recognition, and rewards
Fostering teamwork and collaboration
Enhancing Leadership and Communication
Streamlining processes and workflows
Reducing administrative burden
Optimizing technology
At the system level, some interventions that can help address the broader factors that affect physician burnout include:
Advocating for healthcare reform
Policy change
Regulatory relief
Payment reform
Professional standards
Public awareness
One of the ways to reduce physician burnout is to streamline processes and workflows with technology. Technology can help simplify or eliminate unnecessary or redundant steps or tasks, automate or facilitate non-clinical duties and improve efficiency and quality of care. However, technology can also be a source of frustration and stress if it is not user-friendly, reliable, or efficient.
AI medical scribes are an example of technology that can help streamline processes and workflows. AI medical scribes are software applications that use artificial intelligence to transcribe and document patient encounters. They can capture the conversation between the physician and the patient, extract relevant information, generate clinical notes, and populate the electronic health record. AI medical scribes can help reduce the administrative burden of documentation, save time, improve accuracy, and enhance patient engagement.
According to a study published in JAMA Network Open, AI medical scribes can reduce the time spent on documentation by 18% and increase the time spent on direct patient care by 11%. The study also found that AI medical scribes can improve physicians' documentation satisfaction and reduce burnout symptoms.
AI medical scribes are one of the many examples of how technology can help prevent and reduce physician burnout by streamlining processes and workflows. By using technology wisely and effectively, physicians can focus more on their core mission of providing high-quality patient care.
Physician burnout is a serious problem affecting doctors' and their patient's health and well-being. Multiple factors at different levels cause it and have significant costs and consequences for individuals and organizations. However, it is not inevitable or irreversible. There are effective interventions that can help prevent and reduce physician burnout at different levels, such as streamlining processes and workflows with technology.
One example of technology that can help reduce physician burnout is Tali, an AI ambient scribe and medical dictation that automatically transcribes and documents patient encounters. Tali can help you save time, improve accuracy, enhance patient engagement, and reduce documentation stress. Tali is easy to use, reliable, and secure.
If you want to try Tali for free, visit our website and sign up today. Tali can help you rediscover the joy of medicine and improve your health and happiness. Don't let burnout get the best of you. Try Tali today and see the difference for yourself.
Physician burnout is a prevalent and concerning issue within the medical field, manifesting through emotional exhaustion, depersonalization, and diminished personal accomplishment. According to a survey conducted by the American Medical Association, recent data from 2021-2022 reveals that nearly 63% of physicians reported experiencing at least one symptom of burnout, representing a substantial increase compared to previous years. The survey also indicated a decline in work-life balance satisfaction, with only 30% of doctors feeling content, down from 43% five years earlier.
Physician burnout demonstrates variability across medical specialties. Analysis of the AMA survey data exposed differing burnout rates among specialties, with critical care, rheumatology, infectious diseases, emergency medicine, and neurology registering higher burnout rates, reaching up to 75%. Conversely, specialties such as ophthalmology, dermatology, pathology, orthopedics, and psychiatry showed lower rates, around 45%. The survey further demonstrated that certain specialties experienced significant burnout increases from 2017 to 2021-2022, while others experienced slight decreases, underscoring the unique dynamics influencing burnout within each field.
Physician burnout has far-reaching consequences that extend beyond individual well-being, impacting the healthcare system as a whole. Studies indicate significant financial costs, with estimates suggesting that physician burnout costs the U.S. healthcare system billions annually due to reduced productivity, heightened turnover, and early retirements. Additionally, the quality of patient care is compromised, as burnout correlates with increased medical errors and higher malpractice risk. Burnout is also associated with elevated risks of depression, suicidal ideation, and suicide among physicians, emphasizing the urgent need for comprehensive interventions to address this critical issue.