HIPAA Compliance: What You Need to Know Before Choosing a Health Solution
Table of Contents
Data security and patient privacy are essential aspects of healthcare that affect every physician and clinic authority. With the increasing adoption of telehealth, cloud computing and other technologies, the risk of cyberattacks and data breaches is also growing. Therefore, ensuring that your health solutions comply with the Health Insurance Portability and Accountability Act (HIPAA) is vital. This federal law protects the confidentiality and security of health information.
HIPAA compliance is not only a legal obligation but also a competitive advantage. By choosing HIPAA-compliant health solutions, such as electronic health records (EHR) systems or AI medical scribes, you can enhance your quality of care, improve efficiency, and increase patient satisfaction. In this blog post, we will explain what HIPAA is, how it applies to different health solutions, and what steps you need to take to achieve HIPAA compliance.
What is HIPAA?
HIPAA stands for the Health Insurance Portability and Accountability Act of 1996, a landmark legislation that aims to safeguard patient information in the healthcare industry. HIPAA has two main components: the Privacy Rule and the Security Rule.
The Privacy Rule establishes the standards for using and disclosing protected health information (PHI), which is any information that can identify a patient or relate to their health condition, treatment, or payment. The Privacy Rule grants patients certain rights over their PHI, such as access, amendment, and consent. The Privacy Rule also requires healthcare providers and other covered entities to obtain patient authorization before disclosing PHI for purposes other than treatment, payment, or healthcare operations.
The Security Rule sets the requirements for the protection of electronic PHI (ePHI), which is any PHI created, received, maintained, or transmitted electronically. The Security Rule requires covered entities and their business associates to implement administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of ePHI. The Security Rule also requires covered entities and business associates to conduct risk assessments and adopt security policies and procedures.
The key objectives of HIPAA are to protect patient privacy, ensure data security, and promote standardization in healthcare. HIPAA compliance is enforced by the Office for Civil Rights (OCR) within the Department of Health and Human Services (HHS). OCR conducts audits and investigations of covered entities and business associates and imposes civil and criminal penalties for HIPAA violations.
HIPAA Compliance and Health Solutions
HIPAA compliance is relevant for any health solution that involves the use or disclosure of PHI or ePHI. One of the most common health solutions physicians and clinic authorities use is the EHR. An EHR is a digital version of a patient's medical record that can be shared across different healthcare settings. EHRs can improve care quality, efficiency, and coordination by providing accurate, complete, and timely information.
However, EHRs also pose significant challenges to HIPAA compliance. EHRs must meet the requirements of both the Privacy Rule and the Security Rule. This means that EHRs must:
Implement administrative, physical, and technical safeguards to protect ePHI from unauthorized access or disclosure
Conduct risk assessments and update security measures as needed
Train staff members on privacy and security practices and responsibilities
Establish agreements with business associates that specify their obligations regarding PHI and ePHI
Respond to patient requests regarding their rights over their PHI and ePHI
Report breaches of PHI or ePHI to patients and OCR
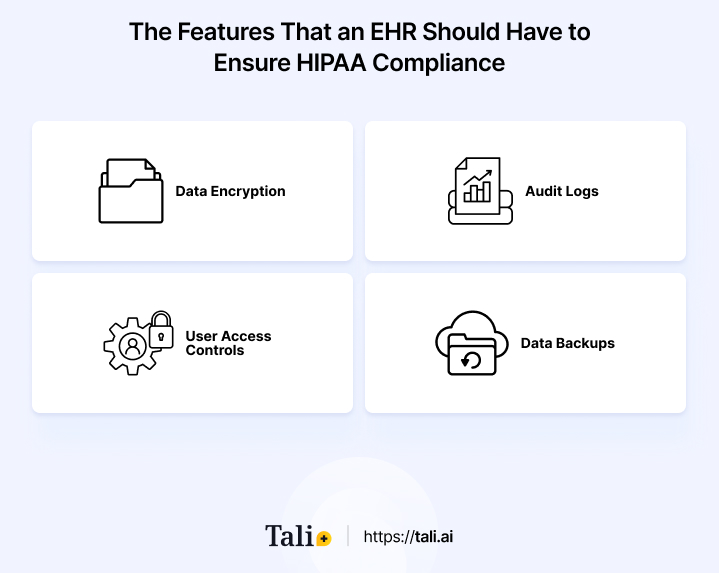
Therefore, choosing an EHR vendor that prioritizes HIPAA compliance and offers robust security features is important. Some of the features that an EHR should have to ensure HIPAA compliance are:
Data encryption: This process transforms data into an unreadable format that can only be accessed with a key. Data encryption can prevent unauthorized access or disclosure of ePHI in case of theft, loss, or hacking.
Audit logs: These records track user actions involving ePHI, such as who accessed what data, when, where, how, and why. Audit logs can help monitor and detect suspicious or inappropriate activities involving ePHI.
User access controls: These mechanisms limit user access to ePHI based on their role, function, or need. User access controls can prevent unauthorized access or disclosure of ePHI by restricting who can view, edit, delete, or share data.
Data backups: These are copies of data stored in a separate location from the original data. Data backups can help restore ePHI in case of loss or damage due to natural disasters, power outages, system failures, or human errors.
Another health solution that can benefit physicians and clinic authorities is the AI medical scribe. An AI medical scribe is software that documents the encounter between a provider and a patient in real time using an EHR. AI medical scribes can improve the quality of care by allowing providers to focus more on the patient rather than on documentation. AI medical scribes can also improve the efficiency of care by reducing documentation time and errors.
However, AI medical scribes also pose potential risks for HIPAA compliance. AI medical scribes must comply with the Privacy and Security rules when using or disclosing PHI or ePHI. This means that AI medical scribes must:
Implement administrative, physical, and technical safeguards to protect ePHI from unauthorized access or disclosure
Conduct risk assessments and update security measures as needed
Train and educate staff on privacy and security practices and responsibilities
Establish agreements with business associates that specify their obligations regarding PHI and ePHI
Report breaches of PHI or ePHI to patients and OCR
Therefore, choosing an AI medical scribe vendor prioritizes HIPAA compliance and offers robust security features is important. Some of the features that an AI medical scribe should have to ensure HIPAA compliance are:
Voice recognition: This is a technology that converts speech into text. Voice recognition can improve the accuracy and efficiency of documentation by allowing providers to dictate rather than type.
Natural language processing: This technology analyzes and interprets natural language. Natural language processing can improve the quality and consistency of documentation by extracting relevant information from speech or text and generating structured data.
Artificial intelligence: This is a technology that mimics human intelligence and learning. Artificial intelligence can improve the effectiveness and safety of documentation by providing feedback, alerts, suggestions, or corrections based on clinical guidelines and best practices.
Common HIPAA Violations and Consequences
HIPAA violations are any actions or omissions that breach the Privacy or Security Rule. HIPAA violations can occur due to negligence, ignorance, malice, or accident. Some common HIPAA violations are:
Unauthorized disclosure: This is when PHI or ePHI is disclosed to a person or entity that is not authorized to receive it. For example, sending an email containing PHI to the wrong recipient, posting PHI on social media, or leaving PHI unattended in a public place.
Improper disposal: This is when PHI or ePHI is disposed of without ensuring its destruction or erasure. For example, throwing away paper records containing PHI in a regular trash bin, donating devices containing ePHI without wiping them clean, or shredding documents containing PHI without using a cross-cut shredder.
Lack of risk assessment: This is when covered entities or business associates fail to conduct regular risk assessments to identify and address potential threats and vulnerabilities to PHI or ePHI. For example, not performing security audits, not updating security software, or not reviewing security policies and procedures.
Insufficient training: This is when covered entities or business associates fail to train their staff on privacy and security practices and responsibilities. For example, not providing privacy and security awareness programs, not testing staff members on their knowledge, or not enforcing sanctions for non-compliance.
HIPAA violations can have serious consequences for covered entities, business associates, and patients. The consequences of HIPAA violations can include the following:
Financial penalties: OCR can impose civil monetary penalties for HIPAA violations ranging from $100 to $50,000 per violation, depending on the level of culpability and the extent of harm. The maximum yearly penalty for repeated violations of the same provision is $1.5 million. In addition, the Department of Justice can also pursue criminal charges for HIPAA violations involving fraud, theft, or malicious intent, resulting in fines of up to $250,000 and imprisonment of up to 10 years.
Reputational damage: HIPAA violations can damage the reputation and trust of covered entities, business associates, and their patients. HIPAA violations can result in negative publicity, loss of customers, loss of partners, loss of revenue, or loss of accreditation.
Legal liability: HIPAA violations can expose covered entities and business associates to legal liability from patients or other parties who have suffered harm or injury due to the breach of PHI or ePHI. HIPAA violations can result in lawsuits, settlements, judgments, or injunctions.
Steps to Achieve HIPAA Compliance
Achieving HIPAA compliance is not a one-time event but a continuous process that requires ongoing monitoring and improvement. Here are some steps that physicians and clinic authorities can take to achieve HIPAA compliance:
Conduct a thorough risk assessment: This is the first and most important step to identify and address potential threats and vulnerabilities to PHI or ePHI. A risk assessment should cover all aspects of the organization, such as people, processes, systems, devices, locations, and partners. A risk assessment should also evaluate the likelihood and impact of each threat and vulnerability and prioritize the actions to mitigate them.
Develop and implement HIPAA policies and procedures: This is the second step to establishing the rules and guidelines for using and disclosing PHI or ePHI within the organization. HIPAA policies and procedures should be based on the requirements of the Privacy Rule and the Security Rule, as well as the risk assessment findings. HIPAA policies and procedures should also be documented, communicated, and enforced throughout the organization.
Train and educate staff members on HIPAA regulations: This is the third step to ensure that all staff members who handle PHI or ePHI are aware of their roles and responsibilities regarding privacy and security. Training and education should cover the basics of HIPAA, the organization’s policies and procedures, the rights of patients, the best practices for protecting PHI or ePHI, and the consequences of non-compliance. Training and education should also be updated regularly and tested periodically.
Regularly monitor and update security measures: This is the fourth step to ensure the organization's security measures are effective and current. Security measures should include administrative, physical, and technical safeguards to protect PHI or ePHI from unauthorized access or disclosure. Security measures should also be monitored regularly using audit logs, activity reports, security audits, or other tools. Security measures should also be updated based on technological changes, regulations, or threats.
Establish a breach response plan and incident reporting process: This is the fifth step to prepare for and respond to any breaches of PHI or ePHI that may occur. A breach response plan should outline the roles and responsibilities of staff members in case of a breach, the steps to contain and investigate the breach, the steps to notify patients and OCR of the breach, and the steps to prevent future breaches. An incident reporting process should enable staff members to promptly and securely report any suspected or actual PHI or ePHI breaches.
Conclusion
HIPAA compliance is a crucial aspect of healthcare that affects every physician and clinic authority who uses or discloses PHI or ePHI. By complying with HIPAA regulations, you can protect your patient's privacy and data security, as well as your reputation and liability.
One way to achieve HIPAA compliance is to choose health solutions designed with privacy and security in mind. One such health solution is Tali, an AI medical dictation and ambient scribe tool that can greatly assist healthcare professionals.
Tali allows you to document patient encounters using voice recognition, natural language processing, and artificial intelligence. Tali also ensures HIPAA compliance by encrypting your data, limiting user access, and providing audit logs. Tali can help you improve your quality of care, efficiency, and patient satisfaction by reducing your documentation burden and allowing you to focus more on your patients.
If you want to experience the benefits of Tali, you can sign up for a free trial today. Tali is easy to use, compatible with any EHR, and affordable for any practice size. Take advantage of this opportunity to transform your healthcare documentation with Tali.
FAQ
HIPAA, or the Health Insurance Portability and Accountability Act, is a critical law safeguarding patient information in healthcare. It consists of the Privacy Rule and the Security Rule. The Privacy Rule governs the use and disclosure of protected health information (PHI), giving patients rights over their PHI. The Security Rule outlines requirements for safeguarding electronic PHI (ePHI). The main goals are patient privacy, data security, and standardization. The Office for Civil Rights enforces HIPAA, conducting audits and imposing penalties for violations.
HIPAA compliance is essential for health solutions involving PHI or ePHI, such as Electronic Health Record (EHR) systems and AI medical scribes. EHRs offer improved care coordination and quality but must follow the Privacy and Security Rules. They need safeguards, risk assessments, staff training, agreements with associates, and breach handling. AI medical scribes, recording patient encounters in real-time, offer efficiency gains but also require adherence to HIPAA. Both solutions benefit from vendors prioritizing compliance and security features.
Common HIPAA violations include unauthorized disclosure, improper PHI disposal, lack of risk assessment, and inadequate staff training. These violations can lead to financial penalties, reputational damage, and legal liability. Penalties vary and can include civil fines and potential criminal charges. Achieving HIPAA compliance involves continuous efforts, including comprehensive risk assessments, policy and procedure development, staff training, ongoing security monitoring, and breach response planning. Complying with HIPAA safeguards patient privacy, data security, reputation, and legal standing in healthcare.
Documentation and Administrative Tasks?