Documentation and Administrative Tasks?
Imagine you are a doctor who runs a small family practice. You have been using paper charts for years and are comfortable with them. You know your patients well and have a good relationship with them. You don't see the need to change anything.
One day, one of your patients comes in with a severe headache and blurred vision. You suspect he may have a brain tumor and refer him to a neurologist. You print out his record and hand it to him, hoping he will bring it to his appointment.
A few weeks later, you get a call from the neurologist. He tells you that your patient has, indeed, a brain tumor, and he needs surgery as soon as possible. He also tells you that he had to run several tests and scans because he didn't have your patient's record. He says your patient forgot to bring it, and he couldn't access it online. He asks you to fax him the record as soon as possible.
You are shocked and worried. You wonder how this could have happened and how you could have prevented it. Is there a better way to keep and share your patient's information?
This is where EMR and EHR come in.
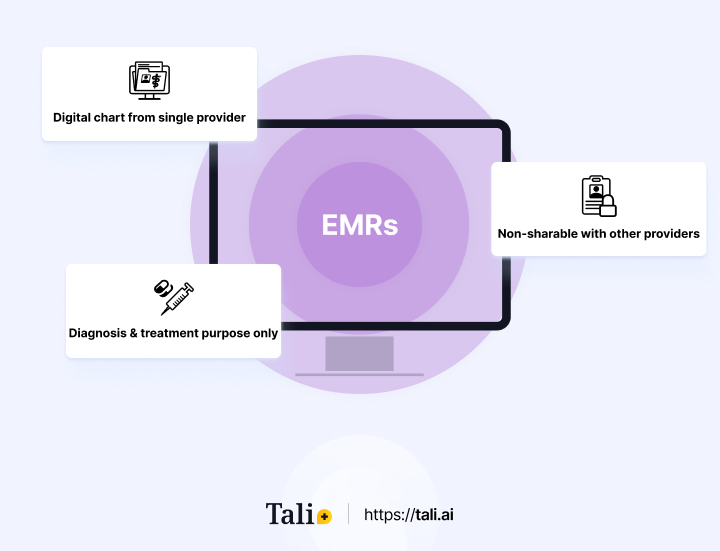
EMR stands for electronic medical record. It is a digital version of the paper chart that contains a patient's medical and treatment history in one practice. An EMR allows you to track data over time, identify which patients are due for preventive screenings or checkups, check how your patients are doing on certain parameters, such as blood pressure or vaccinations, and monitor and improve the quality of care within your practice.
Providers mainly use an EMR for diagnosis and treatment. However, it has some limitations. An EMR is not always designed to easily share information. If your patient sees another provider, such as a specialist or a hospital, you may have to export information, or even print out and fax their record. This can cause delays, errors, or duplication of tests and treatments. An EMR also does not give you a complete picture of your patient's health; it only contains information from your practice.
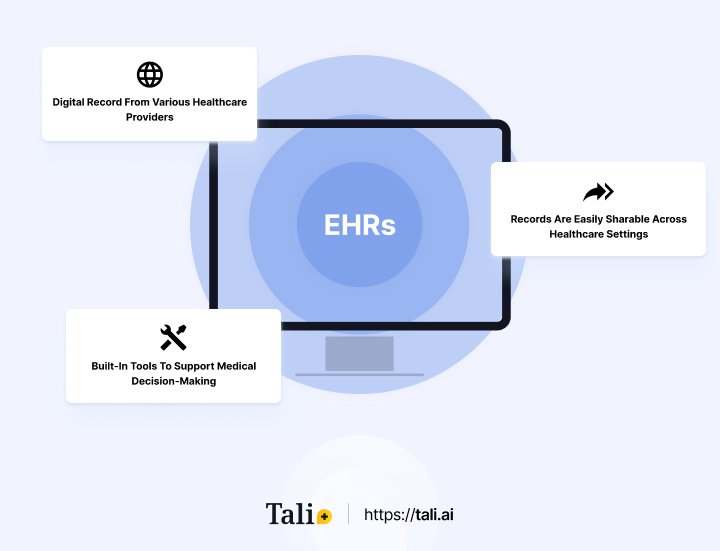
EHR stands for electronic health record. It is a more comprehensive and holistic report of your patient's health. An EHR contains the information from your practice and other providers, labs, imaging centers, pharmacies, and other sources. An EHR allows you to access and share your patient's information with other authorized providers across different settings and locations, coordinate and manage your patient's care more efficiently and effectively, engage your patient in their health and wellness through portals, apps, or devices, support clinical decision making with evidence-based guidelines and alerts, and participate in quality improvement initiatives and reporting.
An EHR is designed to be interoperable, meaning that different systems can exchange and use data. This is important because it enables better provider communication and collaboration, reduces errors and duplication, and improves patient safety and outcomes.
The difference between EMR and EHR may seem subtle – and indeed the terms are often used interchangeably – but it has significant implications for your practice and patients. By adopting an EHR system, you can enhance the quality and continuity of care for your patients, save time and money by reducing administrative tasks and paperwork, increase your productivity and profitability by streamlining workflows and billing processes, improve your compliance with regulations and standards, and gain a competitive edge in the market by offering better services and value to your patients.
EMR has some advantages and disadvantages, depending on your perspective and needs. Here are some of the pros and cons of an EMR:
Improves the quality of care within your practice by allowing you to track data, identify gaps, and monitor outcomes
Reduces the risk of errors, omissions, or illegibility by using standardized formats and templates
Saves time and space by eliminating paper records and filing cabinets
Enhances your security and privacy by using encryption, passwords, and backups
Designed to represent care in a single setting, limiting your ability to create complete picture of your patient’s health
It may require a significant upfront investment in hardware, software, training, and maintenance.
It may not be compatible or interoperable with other systems or standards
EHR has some advantages and disadvantages, depending on your perspective and needs. Here are some of the pros and cons of EHR:
Enhances the quality and continuity of care across the continuum by allowing you to access and share information with other providers or settings
Gives you a comprehensive picture of your patient’s health, as it contains information from multiple sources
Enables better communication and collaboration among providers, reducing errors and duplication
Supports clinical decision-making with evidence-based guidelines and alerts
Allows you to participate in quality improvement initiatives and reporting
Engages your patient in their health and wellness through portals, apps, or devices
This may pose some challenges in terms of security and privacy, as information is shared across different systems or networks.
May be more complex to implement, given the requirements to establish connections with other practices or settings
It may require a change in your workflow or culture, as you need to adopt new standards and protocols.
May encounter some technical issues or glitches, such as downtime, data loss, or interoperability problems
May face some resistance or reluctance from your staff or patients, who may prefer paper records or have concerns about data sharing
The use of EMR and EHR varies across different countries, depending on their health system, policies, standards, and infrastructure. Some countries have more advanced and widespread adoption of EHRs, while others are still developing or implementing it. Here are some examples of how EMRs and EHRs are used in different countries:
Canada has a decentralized health system, with each province or territory responsible for its health services and information systems. There is no national EHR system, but there are several initiatives to promote interoperability and data sharing across jurisdictions. For example, Canada Health Infoway is a non-profit organization that works with federal, provincial, and territorial governments to accelerate the developing and adopting of digital health solutions, such as EHRs. According to a 2020 report by Canada Health Infoway, 85% of primary care physicians use electronic records, and 76% of Canadians have access to at least one digital health service, such as viewing their lab results or booking appointments online. Canadian physicians generally use the name ‘EMR’ to mean both EHRs and EMRs.
The United States has a complex and fragmented health system, with multiple public and private payers and providers. There is no national EHR system, but there are federal incentives and regulations to encourage the adoption and meaningful use of EHRs by eligible providers and hospitals. For example, the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 incentivized providers to adopt certified EHR technology and meet certain criteria for improving quality, safety, efficiency, and care coordination. According to a 2019 report by the Office of the National Coordinator for Health Information Technology (ONC), 86% of office-based physicians use certified EHR technology, and 96% of non-federal acute care hospitals have adopted certified EHR technology.
The European Union (EU) has a diverse range of health systems with different levels of governance, financing, organization, and delivery of health services. There is no common EHR system across the EU, but there are several initiatives to support interoperability and data exchange among member states. For example, the eHealth Network is a voluntary network that brings together national authorities responsible for eHealth to advance cross-border cooperation on digital health services, such as electronic prescriptions and patient summaries. According to a 2020 report by the European Commission, 84% of general practitioners use an EHR system in their practice, and 22% of EU citizens use online health services provided by public authorities.
Understanding the difference between EMRs and EHRs is vital for healthcare professionals seeking to enhance patient care and efficiency. While an EHR offers a more comprehensive approach with its interoperability, managing patient information effectively remains crucial. This is where Tali, an AI medical dictation and ambient scribe tool, can be a game-changer. By utilizing Tali, healthcare providers can streamline documentation, save time, and ensure accurate record-keeping. Tali serves as a reliable virtual assistant, offering numerous benefits such as improved accuracy, reduced administrative burden, and enhanced patient engagement.
Experience the benefits of Tali with our free trial. Tali is not a remote medical scribe service; rather, it provides a cutting-edge alternative that complements your existing workflow. With Tali, you can dictate notes seamlessly during patient interactions, eliminating the need for manual data entry and improving overall efficiency. Don't miss out on the opportunity to revolutionize your practice with this innovative AI tool. Embrace the power of Tali and take your patient care to new heights. Try Tali today and witness the transformation in your practice firsthand.
EMRs (Electronic Medical Records) and EHRs (Electronic Health Records) are both digital versions of patient medical information, but they serve different purposes and have varying levels of functionality. An EMR is a digital version of a paper chart and contains a patient's medical and treatment history within a single practice. It allows healthcare providers to track data over time, monitor patient parameters, and improve care quality within their practice. However, an EMR has limitations when it comes to sharing information with other providers or facilities. On the other hand, an EHR is a more comprehensive and interoperable record that includes information from various sources such as providers, labs, imaging centers, pharmacies, and more. EHRs allow authorized providers to access and share patient information across different settings and locations, enhancing care coordination, reducing errors, and supporting clinical decision-making.
While the terms EMR and EHR are often used interchangeably, understanding the difference between them is crucial for healthcare professionals and their patients. Adopting an EHR system offers numerous benefits, including improved patient care quality, reduced administrative tasks, increased efficiency, better compliance with regulations, and a competitive advantage in the market. EHRs enable seamless communication and collaboration among providers, comprehensive patient health insights, evidence-based decision support, and patient engagement through portals and apps. In contrast, EMRs may lead to limitations in data sharing, potential errors or duplication, and a less comprehensive view of a patient's health.
Both EMRs and EHRs have advantages and disadvantages. EMRs improve care quality, reduce errors, and save time by eliminating paper records. However, they might limit the complete picture of a patient's health and require manual sharing of information, potentially causing delays or errors. EHRs enhance care continuity, offer comprehensive health insights, and improve collaboration among providers. They support clinical decision-making, engage patients, and participate in quality improvement initiatives. Nonetheless, EHRs may pose security challenges, require more complex implementation, and encounter technical issues. Additionally, transitioning to EHRs might involve changes in workflow and meet resistance from staff and patients. Careful consideration of these factors is essential when choosing between EMRs and EHRs for a healthcare practice.